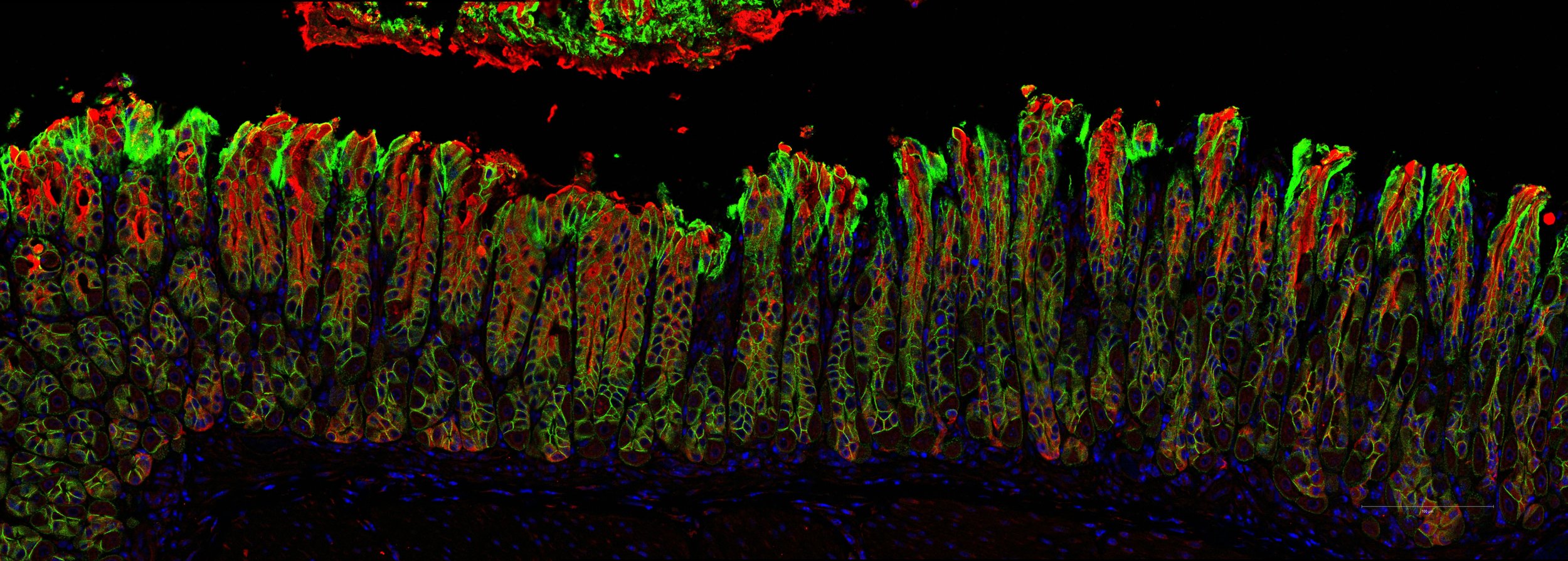
The Lencer laboratory studies the cell and molecular biology of polarized epithelial cells lining mucosal surfaces.
The projects focus on how barrier epithelial cells interact with the lumen and sub-epithelial microenvironment, and on the biology of bacterial toxin pathogenesis and mucosal host defense.
Our Mission
Our lab is dedicated to fostering an environment where scientific progress thrives. Composed of a diverse team of highly skilled and experienced scientists, we bring a range of expertise to the table, enabling us to approach complex challenges from different angles. We believe that collaboration is key to unlocking groundbreaking discoveries, and our lab is built on a foundation of problem solving and collective intelligence. Our commitment to excellence is reflected in everything we do, from conducting rigorous experiments to ensuring the highest standards of research integrity. Together, we aspire to make a meaningful impact on the scientific community and society as a whole, elevating the pursuit of knowledge to new heights.Projects
-

The PARD6B and Apical Endosome research programs
We discovered that upon virus or enterotoxin binding to glycosphingolipid receptors on the apical membrane of barrier epithelial, the host cell rapidly degrades the PARD6B-aPKC-Cdc42 polarity complex to down-regulate the apical endosome. This blocks further entry of the invading toxins and viruses in a novel form of cell autonomous host defense.
-

The IBD risk gene INAVA (C1ORF106) research programs
The lab aims to elucidate how the IBD-risk gene C1ORF106/INAVA acts in human intestinal epithelia to manage environmentally-induced cell stress, inflammation, and the integrity of mucosal surfaces. We found that INAVA exhibits dual activities mechanistically linking epithelial barrier function and inflammatory signaling by IL1β.
-

The GM1 glycosphingolipid research programs
We found the structure of the ceramide domain of the cholera toxin’s GM1 glycosphingolipid receptor plays a decisive role in the trafficking of the toxin. The discovery describes a general rule for glycosphingolipid sorting by eucaryotic cells and may have clinical applications for design of ceramide-based vehicles enabling mucosal delivery of peptide and protein biologics and their amplified biodistribution.
-

The Endoplasmic Reticulum and ER stress research programs
We found that upon entry into the endoplasmic reticulum (ER) of host cells, a portion of these toxins activate the unfolded-protein sensor IRE1α. And we discovered the structural basis for unfolded protein recognition by IRE1a leading to induction of the unfolded protein response. Our work on IRE1a led to a new project focused on the biology of its evolutionarily evolved paralogue IRE1b.
-

The FcRn and IgG Trafficking research programs
In another project, the lab studies the cell and molecular biology of transcytosis by the MHC Class I-like IgG receptor FcRn. FcRn transports IgG across mucosal surfaces where it may function in immune surveillance and host defense. The transcytotic pathway across barrier epithelial cells provides a critical link between the outside (microbial) and inside (sterile) worlds of the gut (and other mucosal surfaces lining the respiratory and genitourinary tracts). Our work has elucidated the itinerary and many genes operating in this pathway.
-

Gut-Brain Axis and Microbiome Signaling research programs
Our lab conducts basic and translational gastroenterology research. This project is specifically interested in how gut microbes might affects hunger, satiety, and food choice. Our research is done in collaboration with a team of scientists and clinicians at both Boston Children’s Hospital and Dr. Eric Alm’s lab at MIT who focus on the interaction between gut microbes, the gastroenterology tract, and the brain.
Harvard Immunology PhD Program
Boston Children’s Hospital Division of Gastroenterology, Hepatology and Nutrition
Harvard Digestive Disease Center